GenAI provides hope for an equitable healthcare revolution, but advances in technology must never come at the cost of patient rights
The next generation of ethical Generative Artificial Intelligence (GenAI) provides new hope for an equitable healthcare revolution – but technological advances must never come at the cost of patient rights.
This was the consensus amongst top African and American health AI experts who participated in a webinar about the impact of GenAI on healthcare, hosted by Vantage Health Technology – part of BroadReach Group, a social enterprise focussed on health equity globally.
-
Sale!
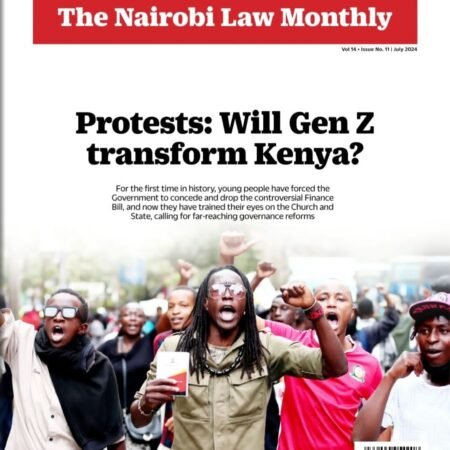
Download Nairobi Law Monthly Magazine July 2024 Edition
Downloads Original price was: KShs200.00.KShs100.00Current price is: KShs100.00.
“The fundamental issue in healthcare anywhere in the world is that demand outstrips supply regarding health services, doctors, nurses, and medications. In Sub-Saharan Africa, for instance, there are 0.2 doctors per 1000 people,” explains Dr John Sargent, co-founder of the BroadReach Group.
He says we are trying to deliver on an antiquated “sick care” model, with a certain ratio of doctors to patients. “We need to change this paradigm to be more effective by matching the supply and demand sides of our health systems in new digital ways,” says Dr Sargent.
While GenAI has the potential to revolutionise how healthcare supply and demand are balanced, it is not the be-all-and-end-all of health tech. “The aim is not to get distracted by a shiny new toy – we need to put the patient first by protecting privacy and training our models against bias. We must always remember that technology is just a tool in service of patient care and supporting the healthcare workforce to improve health outcomes.”
Using GenAI to tackle specific diseases such as HIV and AIDS
Jaya Plmanabhan, chief scientist at innovation consultancy Newfire Global who trains health AI models, says he is particularly excited about how large language models could be trained to revolutionise virtual expertise on diseases such as HIV and AIDS.
“We call these ‘Role Specific Domain Models, ’ and they have the potential to be programmed to know everything about a particular disease, to better guide healthcare professionals on how to treat patients. This is a tremendously exciting prospect in the mission to end new HIV infections by 2030.”
These Private Language Models (PLMs) become oracles on a subject and are especially useful in helping solve hard problems in HIV management, such as loss to follow-up – a term for patients who drop off treatment.
“Trying to find patients is critical to ensure they don’t become resistant to drugs due to skipping doses. We can make our outreach much more engaging through conversational messages in their mother tongue, which can help us get people back into the clinic and back into care,” explains Ruan Viljoen, Chief Technology Officer of the BroadReach Group.
Start with the problem, not the solution
“There is a quote that says we should fall in love with the problem, not the solution, which in this case is AI,” says Viljoen. “I believe the biggest challenge is still health inequity – healthcare access can vary depending on race, location, or age.”
Viljoen said GenAI can help solve practical problems, such as overburdened frontline healthcare workers and lack of time. “What are the repetitive, administrative tasks that are stealing their time? For instance, GenAI can help nurses with automated note-taking in patient interviews, relieving an administrative burden. The goal is not to replace the role but to free up their time for value-added work.”
One of the greatest uses of AI in health is to help healthcare workers focus on the next best action. “We can use large datasets and extract insights to help healthcare workers, delivered via easy-to-digest and secure messaging like emails or text messages. This is nothing new – we’ve done this in some form for nearly a decade using our AI-enabled platform, Vantage. What I’m most excited about, is how we can augment the quality of the interactions to bring together human and artificial intelligence.”
Heeding the risks and creating guardrails
The top ethical considerations for AI in healthcare are privacy, accuracy, and fairness. She urged all AI systems to start with guardrails and ethics within their foundational design.
“There is a perception that there are no regulations for the use of AI in healthcare, but to assume we are operating in the wild west is not true,” says Vedantha Singh, an AI ethics in healthcare researcher and virologist from the University of Cape Town. “International bodies are sharing guidelines, and regulation is slowly evolving – including in Africa. Egypt, Rwanda and Mauritius already have strong AI policies.” This includes emphasising human labour not being completely replaced and giving patients agency over how their data is used.
Companies must embed ethical guardrails in their health products; while GenAI can reduce costs and personalise care, it must be used carefully. For example, if the data is biased, the model will be biased. GenAI can also create fake patient profiles to commit fraud. Unbiased, quality data compliant with regulations such as HIPAA and POPIA or GDPR must be prioritised.
“We need to stay committed to immovable core principles – we cannot compromise on the human in the middle of it all.”
Reaching the hardest-to-reach patients
GenAI is not just improving healthcare for urban patients. Those in deeply rural areas could benefit too.
“Internet connectivity and satellite communication are becoming more ubiquitous. A few things provide hope: Big cloud providers are providing more ‘edge computing’ for rural areas, the mobile phone is becoming a very powerful computer in the pockets of people all around the world, and small rural clinics can use smaller GenAI models which require smaller amounts of data and computing power– they don’t need to use ChatGPT,” says Viljoen.
GenAI can increase affordable and equitable healthcare through the automation of routine tasks. To create a world where more equitable healthcare exists, it is critical to establish strong partnerships between donors, policymakers, researchers, and healthcare implementers.